Pear's Medicaid Primer (Part 1)
This episode is part of Pear VC's series on Medicaid, covering the basics that founders need to know to build innovations that support communities in need.
Subscribe to our substack for updates and listen on Apple Podcasts or Spotify.
Welcome back to the Pear Healthcare Playbook! Every week, we’ll be getting to know trailblazing healthcare leaders and diving into building a digital health business from 0 to 1.
Why are we writing this?
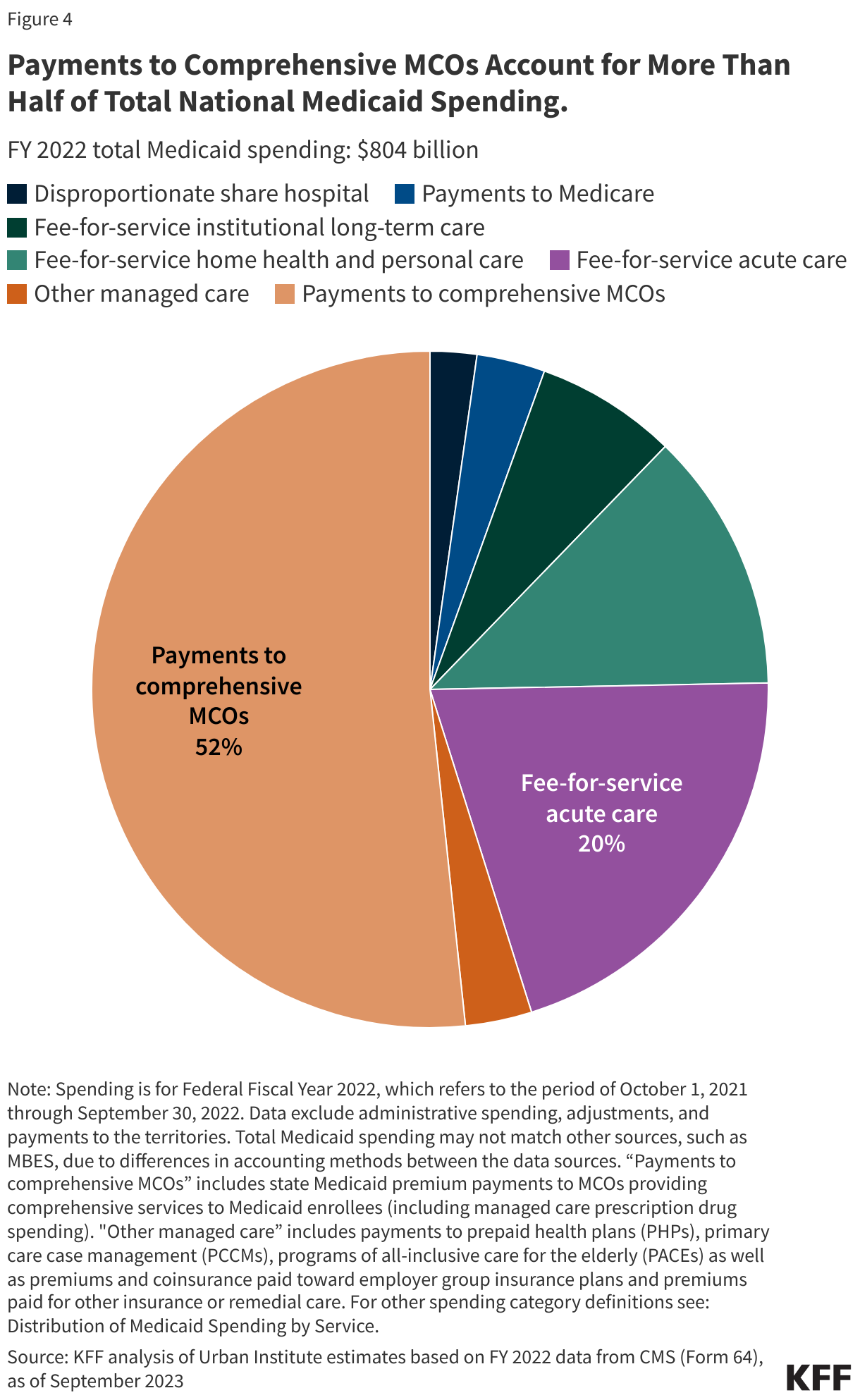
In recent decades, Medicaid innovation has significantly increased, due to the growth of managed care. With over 70% of Medicaid beneficiaries now enrolled in managed care plans, these plans have financial incentives to boost quality and reduce costs which has counterbalanced the low reimbursement rates that had previously discouraged many startups.
Furthermore, Medicaid covers nearly 25% of Americans, with 83 million lives, including 7 million children through the Children's Health Insurance Program (CHIP) (Source). Medicaid also covers 40% of all births in the United States (Source). Given the large number of beneficiaries needing improved access to care, Medicaid presents a compelling investment opportunity.
Investors like Pear VC are eager to identify these opportunities. However, we understand the challenges that healthcare founders, especially those from different industries, face in grasping the complexities of Medicaid. In this series, we aim to highlight experts' and operators' perspectives on building in the Medicaid space. We'll begin with high-level perspectives from federal and state agencies, Federally Qualified Health Centers (FQHCs), and managed care organizations. We will then delve into the approaches of successful founders.
This series will be broken up into many individual posts. The first of these posts is an initial primer which aims to guide founders through the myriad of actors, acronyms, programs, and the research and innovation landscape. We aim to refine this resource over time. Please note, all content reflects the authors' opinions. Stay tuned for following posts where we interview different folks and discuss their insights.
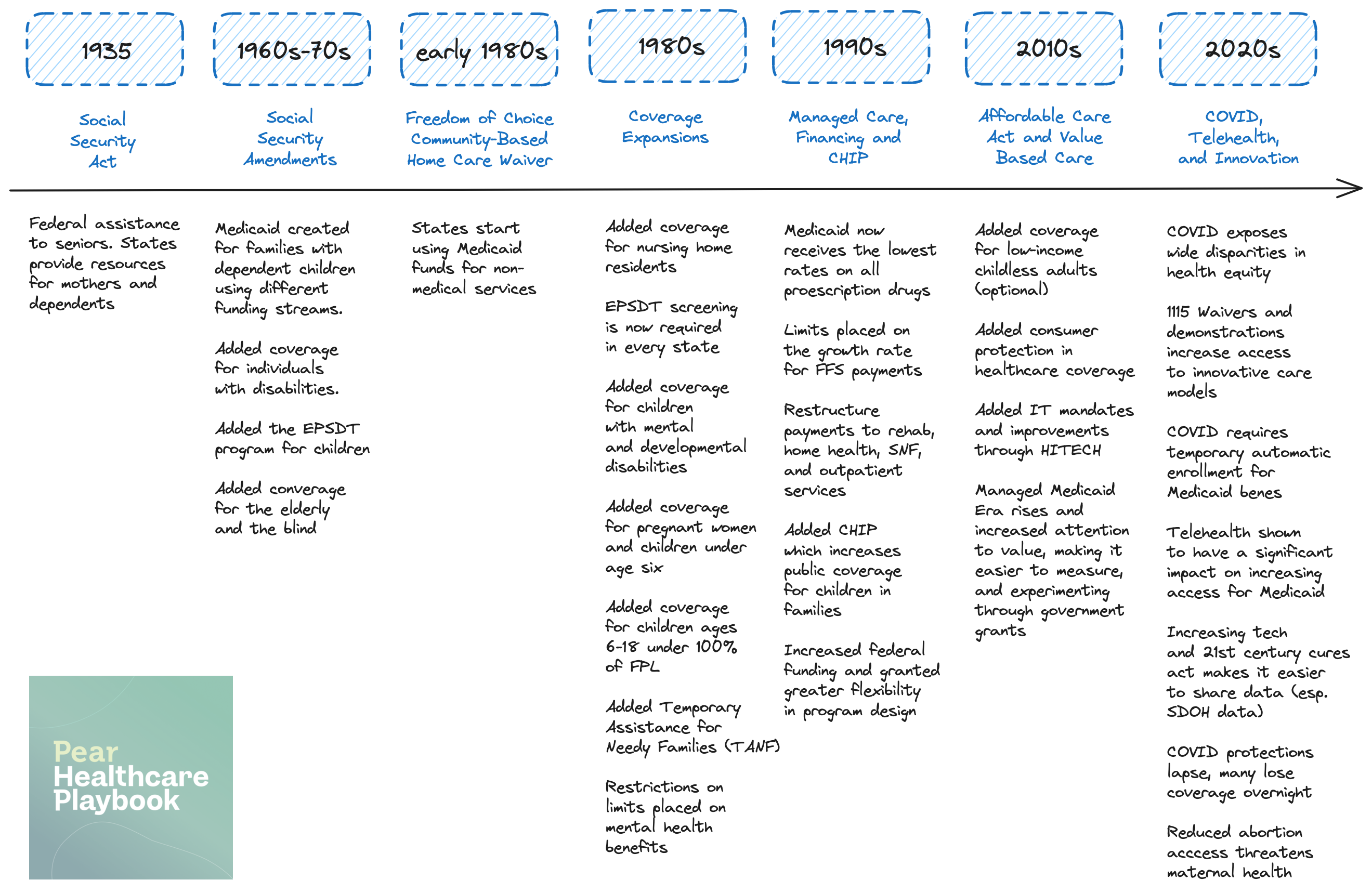
History
Medicaid is a patchwork series of programs administered by state agencies, catering to niche populations that has evolved and increased in scope over time. [History]
Glossary of Actors, Acronyms and Programs
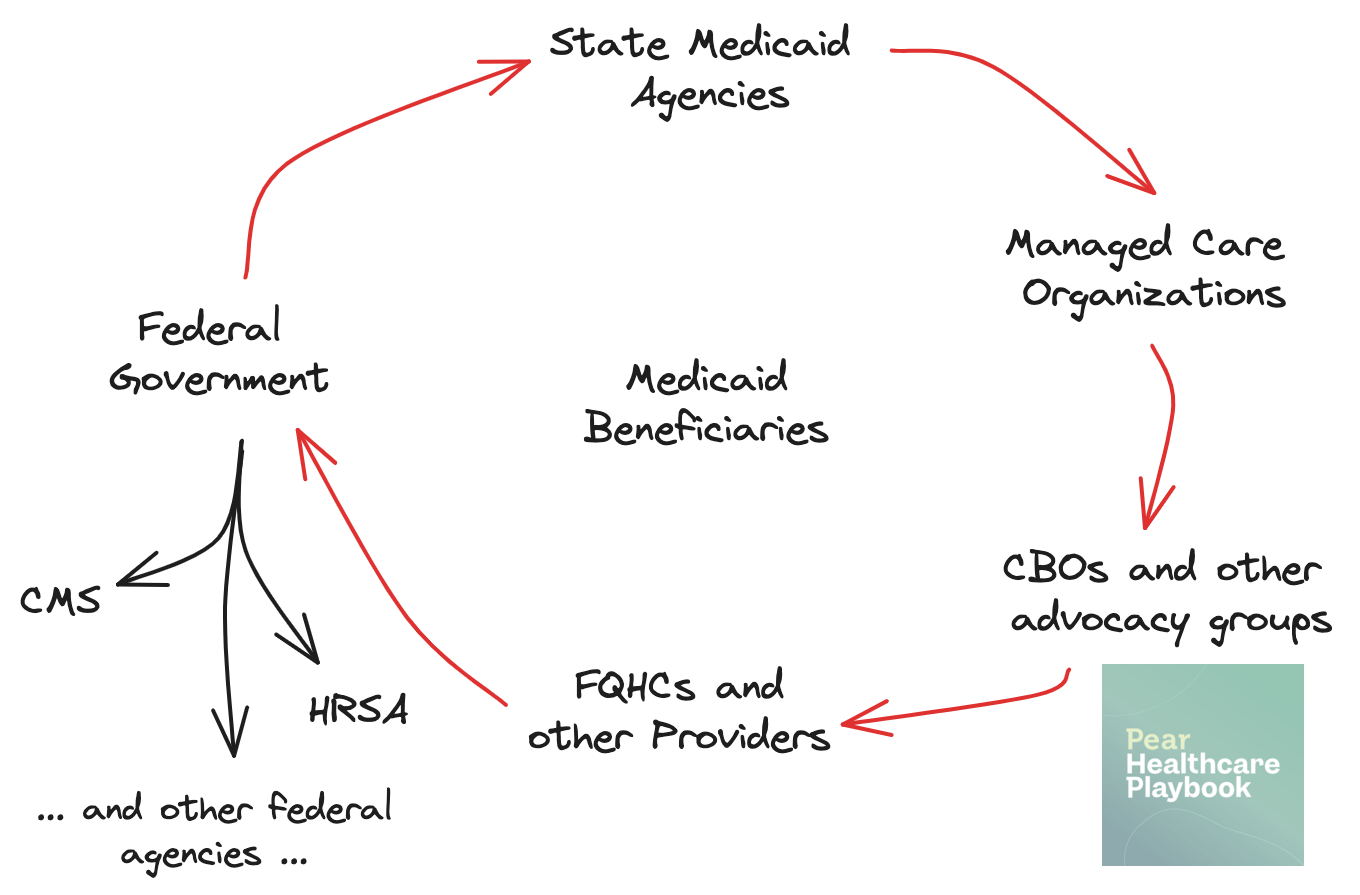
Federal Level
All the federal agencies listed here roll up into the Department of Health and Human Services (HHS). Led by Xavier Becerra, HHS has twelve operating divisions and manages nearly $1.8 trillion dollars in annual budget (Source)
Centers for Medicare & Medicaid Services (CMS) oversees the Medicaid program nationally, setting broad guidelines, regulations, and providing federal funding.
Center for Medicare & Medicaid Innovation (CMMI) is a division within CMS that develops and tests new payment and service delivery models to reduce costs and improve quality in Medicare, Medicaid, and CHIP. CMMI’s initiatives often target areas with significant room for improvement or high costs, such as chronic diseases or behavioral health. By testing new approaches at the state level, CMMI identifies strategies that can be scaled nationally through CMS. This collaboration enhances healthcare delivery and reduces costs, with the federal government ensuring program integrity and innovation while allowing state flexibility.
Health Resources and Services Administration (HRSA) provides funding for healthcare to vulnerable populations and oversees programs like the 340B Drug Pricing Program and Federally Qualified Health Centers (FQHCs).
Advanced Research Projects Agency for Health (ARPA-H) drives transformative innovation in health and biomedical research through high-risk, high-reward projects.
Medicaid Fraud Control Units (MFCUs), in the Office of the Inspector General in HHS, investigate and prosecute Medicaid provider fraud and patient abuse or neglect in healthcare facilities.
Centers for Disease Control (CDC) protects public health by controlling and preventing disease, injury, and disability, and works closely with state Medicaid programs to implement public health initiatives for low-income populations. The CDC also collects useful public health data.
Agency for Healthcare Research and Quality (AHRQ) focuses on improving the quality, safety, efficiency, and effectiveness of healthcare, and developed the first national, standardized survey of patients' perspectives of hospital care (HCAHPS).
Indian Health Service (IHS) provides federal health services to American Indians and Alaska Natives, and operates one of the largest rural telehealth networks in the United States.
National Institutes of Health (NIH) is the primary agency for conducting and supporting medical research, and funds numerous studies aimed at addressing health disparities in Medicaid and low-income communities.
Substance Abuse and Mental Health Services Administration (SAMHSA) improves the quality and availability of substance abuse prevention, addiction treatment, and mental health services, and its National Helpline receives over 300,000 calls each year. They provide critical support to Medicaid beneficiaries and underserved populations through various grants and programs.
Medicaid and CHIP Payment and Access Commission (MACPAC) is a non-partisan legislative branch agency that provides policy analysis and recommendations to Congress, the U.S. Department of Health and Human Services, and states on Medicaid and CHIP, offering independent information through reports on payment, eligibility, coverage, access, quality of care, and program interactions with Medicare and the healthcare system.
State Level
Congress supplies significant funding and guidelines for Medicaid, but each state runs its own program. Federal requirements are detailed in the Social Security Act's Title XIX, with regulations and guidance from CMS.
States are required to meet federal requirements to receive matching funds. They have flexibility in setting eligibility, services, and payment methods, through state plan design, waiver programs, and state-funded programs.
State Medicaid Agencies administer Medicaid programs within their states, developing policies, managing operations, and determining eligibility criteria.
State Legislatures approve state budgets for Medicaid and enact laws that influence Medicaid policies and funding.
Local Level
County and Local Health Departments, delegated by the state government, administer Medicaid services, especially in rural areas. They also deliver direct public health services and manage local health initiatives. Their responsibilities span a wide range of tasks such as disease control, health education, sanitation, and the provision of various health services including maternal and child health, mental health, and home care.
Healthcare Providers
Hospitals and Clinics deliver a range of medical services to Medicaid beneficiaries and participate in managed care or fee-for-service arrangements.
Federally Qualified Health Centers (FQHCs) and Look-Alikes (LALs) provide comprehensive primary and preventive care to underserved communities and are significant Medicaid providers, often serving as a critical access point for many beneficiaries. 1 in every 11 Americans are served by nearly 15,000 FQHCs and LALs across the country.
Critical Access Hospitals and Rural Hospitals serve Medicaid members by providing essential healthcare services to underserved and geographically isolated communities, ensuring access to primary, emergency, and acute care for low-income patients who might otherwise face significant barriers to healthcare access.
Medicaid covers a larger share of the population in rural areas, with 24% of nonelderly individuals and 47% of children receiving coverage, compared to 22% and 40% in urban areas, respectively. It fills gaps in private insurance coverage in rural areas, where fewer jobs offer employer-sponsored insurance, although rural areas still have slightly higher uninsured rates. Additionally, Medicaid is vital for rural maternal health, covering 50% of rural births compared to 41.9% in urban areas.
However, compared to urban hospitals, rural hospitals have a lower percentage of patient days attributed to Medicaid patients.
Physicians and Specialists provide primary and specialty care to Medicaid patients and must enroll in Medicaid to receive reimbursement.
Pharmacies dispense medications to Medicaid beneficiaries and participate in Medicaid’s drug rebate program. 340B Pharmacies participate in the 340B Drug Pricing Program, allowing them to purchase medications at reduced prices to provide affordable medications to underserved and low-income patients.
Community Health Workers (CHWs) play a vital role in linking healthcare services to community members, providing education, support, and advocacy. The Brooklyn Health Home network uses CHWs to help manage the health and social needs of Medicaid beneficiaries.
Managed Care Organizations (MCOs)
Private Insurance Companies contract with state Medicaid agencies to provide managed care services, managing networks of healthcare providers and coordinating care.
States pay managed care plans a fixed, per-member per-month (PMPM) capitation rate to provide comprehensive services to Medicaid enrollees. Plans are at financial risk if costs exceed the capitation payments, incentivizing cost control.
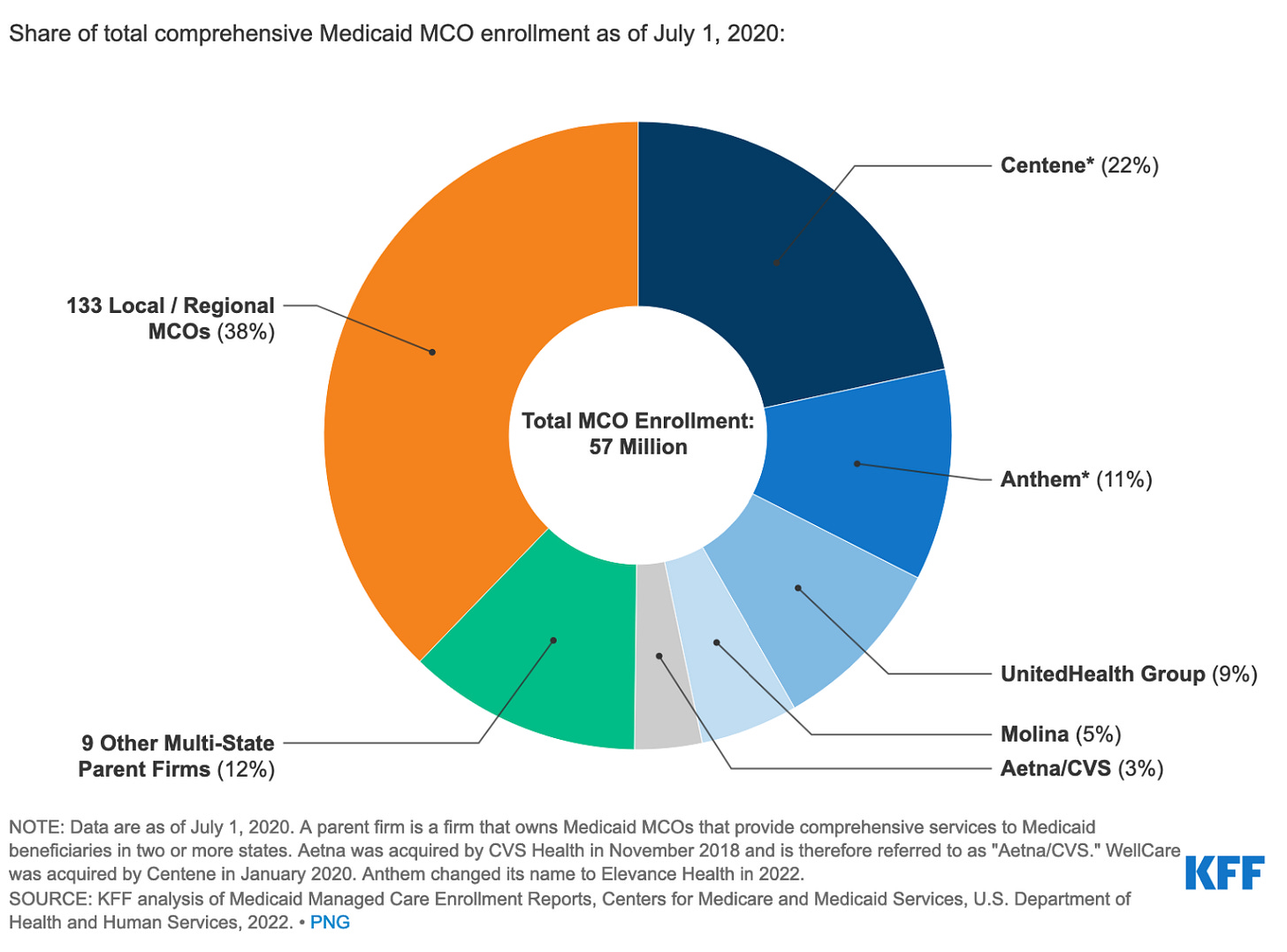
As of 2023, approximately 70% of Medicaid beneficiaries are enrolled in managed care plans. The top five Medicaid MCOs include Centene, Elevance (formerly Anthem), UnitedHealth Group, Molina, and CVS Health, which together account for 50% of Medicaid MCO enrollment nationally.
States may withhold a portion of the capitation payment, which plans can earn back by meeting performance targets related to quality, access, or costs. This incentivizes plans to improve quality and efficiency.
Many states risk-adjust capitation rates based on enrollee health status, providing higher payments for sicker enrollees. This reduces the incentive for plans to avoid high-risk enrollees.
States often exclude services like behavioral health, pharmacy, dental, and LTSS from MCO contracts, assigning them to fee-for-service systems or limited benefit plans.
Support and Advocacy Groups
Community Based Organizations are nonprofits which offer support services, education, and outreach to Medicaid beneficiaries while advocating for their needs.
Patient Advocacy Groups protect the rights and interests of Medicaid beneficiaries, lobbying for policy changes and increased funding.
Some national patient advocacy organizations that work on Medicaid issues include the National Health Council (NHC), Medicare Access for Patients Rx (MAPRx) Coalition, National Minority Health Association (NMHA), National Rural Health Association (NRHA), OutCare (LGBTQ+ health advocacy), and the Rare Disease Diversity Coalition, along with the PAN Foundation itself, which helps patients access and afford healthcare, including those on Medicaid.
Other Organizations
Academic and Research Institutions conduct studies and evaluations to inform policy decisions and program improvements. For example, the Institute for Medicaid Innovation addresses clinical, research, and policy issues in Medicaid, and AcademyHealth manages initiatives like the Medicaid Data Learning Network and MODRN for peer learning and data analysis.
Technology Vendors supply electronic health records systems and other IT solutions to enhance data management and service delivery.
Legal and Policy Experts provide guidance on compliance with regulations and advocate for the legal protections and rights of beneficiaries.
Programs
Medicaid mandatory and optional benefits are described here. The following represent a fraction of the benefits that are available to Medicaid patients.
Early and Periodic Screening, Diagnostic and Treatment (EPSDT) program ensures that children under 21 receive age-appropriate screening and preventative services.
Temporary Assistance for Needy Families (TANF) provides financial assistance and supportive services to low-income families to promote self-sufficiency, and coordinates with Medicaid to ensure healthcare coverage for eligible families.
Children’s Health Insurance Program (CHIP) offers low-cost health coverage to children in families that earn too much to qualify for Medicaid but cannot afford private insurance, ensuring millions of children receive essential healthcare services.
While Medicaid and CHIP are separate programs, they often work together to provide health insurance to low-income children. CHIP provides coverage for uninsured children under 19 years old from families whose income is too high to qualify for Medicaid. Both Medicaid and CHIP are managed by states and comply with federal regulations, with shared funding and regulation from both state and federal governments.
Disproportionate Share Hospital (DSH) Payments provide financial assistance to hospitals that serve a large number of Medicaid and uninsured patients, helping to ensure that these hospitals can continue to offer care to underserved populations.
Long Term Support and Services (LTSS) provide a broad range of medical and personal care services (such as feeding, bathing, dressing, medication management etc) to aging or disabled people in need of such services. An estimated 7.7M people were on LTSS care through Medicaid in 2020 and the US spent nearly 30% of total national and state Medicaid spending on LTSS.
Home and Community Based Services (HCBS) offers opportunities for Medicaid beneficiaries to get services in their own homes or communities instead of institutional or other isolated settings. These programs cater to a variety of targeted population groups, including people with intellectual or developmental disabilities, physical disabilities, and/or mental illnesses. In 2014, 53% of all Medicaid long-term care spending was allocated to home and community-based services.
Key Statistics
Eligibility and Enrollment
The federal government sets mininmum eligibility levels for specific populations. However, states can set eligibility levels higher than federal minimums.

Medicaid coverage has been rising over time since the ACA expansion. During COVID it peaked as Medicaid enrollees were not required to re-apply. [Source]
Eligibility requirements will typically vary by state. States can provide additional support to qualified individuals above the income thresholds set below in this table. This data is reported as of January 2024. [Source]
Mandatory Eligibility Groups
States have flexibility in deciding which Medicaid eligibility groups to cover beyond the mandatory federal requirements. States consider their budgetary situation and priorities when deciding which optional groups to cover.
States are required by federal law to provide Medicaid coverage to certain population groups, such as low-income families, children, pregnant women, the elderly, and individuals with disabilities.
These mandatory groups include children under age 21 not receiving cash, qualified pregnant women and infants, and most individuals receiving Supplemental Security Income (SSI).
Optional Eligibility Groups
Beyond the mandatory groups, states can choose to cover additional "optional" eligibility groups. Covering additional optional groups increases the state's Medicaid costs, but also allows them to leverage federal matching funds.
Common optional groups covered by many states include children and pregnant women above the mandatory income limits, individuals needing long-term care services, and the "medically needy" who have high medical expenses that allow them to "spend down" income to qualify.
The Affordable Care Act gave states the option to expand Medicaid to cover non-elderly adults with incomes up to 133% FPL, which some states have adopted.
Managed Medicaid
Managed Medicaid MCO Enrollment is concentrated in the following top five healthplans which own many local subsidiaries. Managed medicaid plans account for the lion’s share of Medicaid enrollment.
Thanks for reading!
Continue following along to our podcast series on Medicaid weekly! Our next primer post will be on financing. Please feel free to provide any suggestions or corrections to Lipsa Panda.
A note from our sponsor: Banc of California
Looking for guidance, connections, resources, opportunity? Banc of California’s banking products and services are built to support your evolving needs as you navigate the challenges of growing a successful business. As you continue to scale, our team will be with you every step of the way. Ready to take your business to the next level? Learn more:
Thanks for reading Pear Healthcare Playbook! Subscribe for free to receive new posts and support my work.







This is such a great overview and great effort to level set. I am curious about the next ones (part 2 and 3 perhaps) and what you plan to cover? I would love to share some insights as I have been working on this area for over 5 years.