Lessons from Kevin Riddleberger, Co-Founder of DispatchHealth, on Crafting a Trusted and Comprehensive Home Healthcare Experience
Subscribe to our substack for updates and listen on Apple Podcasts or Spotify. Connect with Andrew or Lipsa if you find this post insightful and want to learn more.
Welcome back to the Pear Healthcare Playbook! Every week, we’ll be getting to know trailblazing healthcare leaders and dive into building a digital health business from 0 to 1.
Today, we're so excited to get to know Kevin Riddleberger, Co-Founder of DispatchHealth.
Kevin has over 20 years of experience in both clinical and management roles within the healthcare sector. His passion for transforming healthcare delivery is evident through his focus on technology, process improvement, and enhancing quality standards.
As a board-certified physician assistant, Kevin has contributed his expertise to hospital quality improvement committees and has held the position of president at the Colorado Academy of Physician Assistants. Additionally, he plays a vital role as an advisor in Colorado’s healthcare startup community, where he provides guidance on both business and clinical matters. Prior to his role as co-founder of DispatchHealth, Kevin was responsible for leading clinical solutions and strategy at iTriage.
In this episode, we explore the founding and scaling of DispatchHealth, the challenges of reimbursement and scaling, strategies for securing payer contracts, the provider model they use, their success stories, and legal and fundraising advice for founders.
Note: Kevin did the interview in early 2024 when he was working for DispatchHealth. He has since moved to a different position.
If you prefer to listen:
Starting DispatchHealth
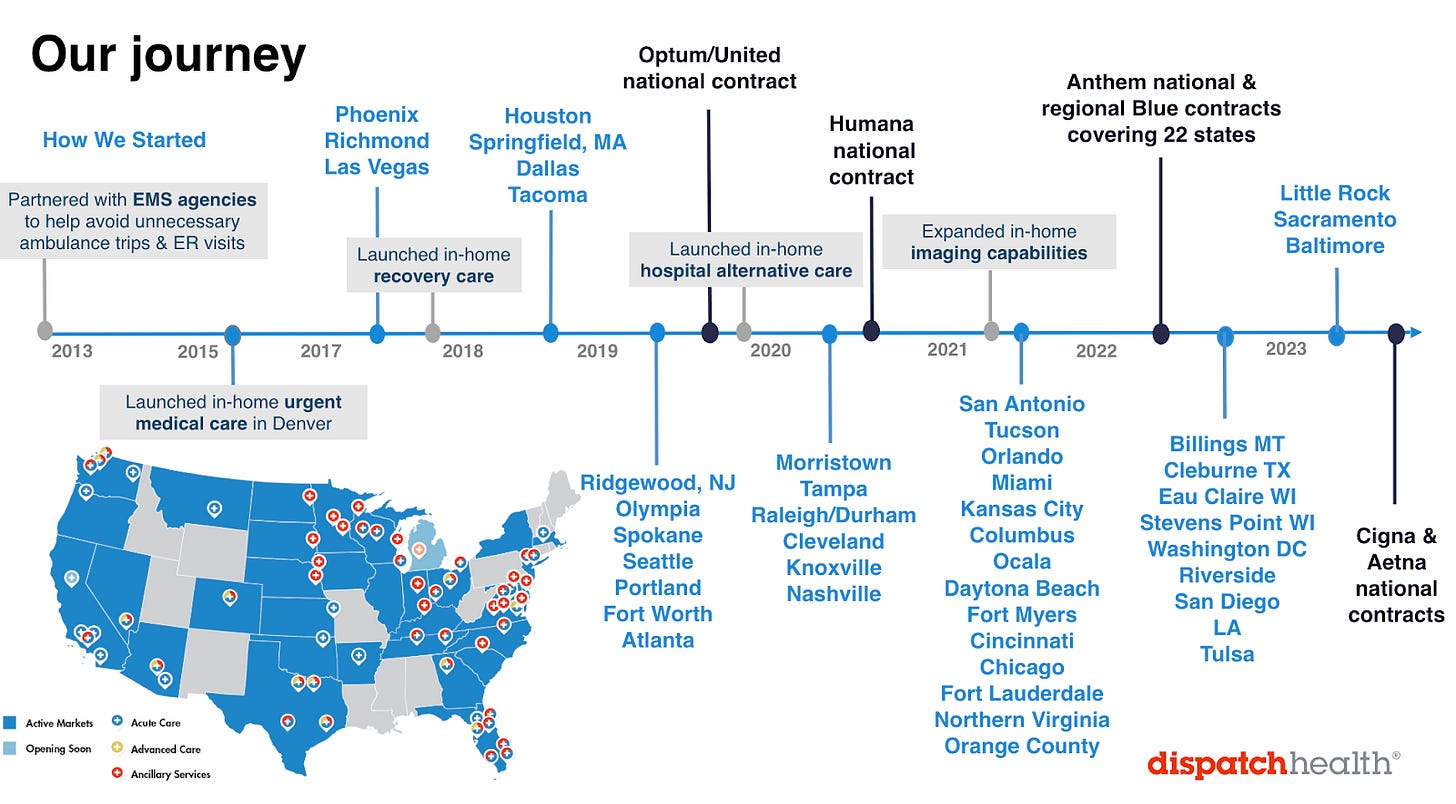
DispatchHealth has been on an impressive journey over the last decade, building the world's largest home care service system. The company achieves this by providing tech-enabled services focused on high-acuity care. This involves intervening in the pre-hospital space to prevent unnecessary emergency department visits, assisting patients in transitioning safely out of hospitals, preventing readmissions, and even hospitalizing patients at home to provide skilled nursing facility-level care. Additionally, they offer last-mile services with portable imaging and ultrasound capabilities.
Kevin Riddleberger and his co-founder Dr. Mark Prather, initially met while working at iTriage, a company that used a mobile app to guide people to the appropriate level of care based on their symptoms. iTriage’s acquisition by Aetna and the evolving market dynamics highlighted the potential to deliver care directly to patients at home.
The founders identified five key factors in 2013 that gave them confidence to build DispatchHealth:
Consumer Adoption: They observed a growing trend in consumer adoption of convenient services in various industries and saw an opportunity to bring this convenience to healthcare by providing home-based services.
Advancements in Technology: Improved technology allowed them to equip vehicles with the necessary tools to handle high-acuity conditions, making home care feasible.
Workforce Utilization: The rise of nurse practitioners (NPs) and physician assistants (PAs) provided a skilled workforce capable of delivering safe and effective home care.
Community Paramedicine: Grant funding was drying up for community paramedicine programs despite the great outcomes they produced. Recognizing the success and challenges of community paramedicine programs, they aimed to create a sustainable business model that could continue to deliver these benefits.
Transition from Fee-for-service (FFS) to Value-Based Care: They saw an opportunity to reduce costs and improve patient outcomes by avoiding expensive facilities like emergency rooms and skilled nursing facilities.
From the very beginning they bootstrapped a partnership with a local EMS agency in Denver called South Metro Fire Rescue and Denver served as their first market.
“Industry statistics showed that about 17% of individuals who call 911 do not need to be transported to the ER. Financially, a typical ambulance ride costs about $1,000, and an ER visit can cost around $2,000. These are expensive services, especially for cases that could be treated at home.”
By treating these patients in the comfort of their home, DispatchHealth could save costs associated with ambulance rides and ER visits while providing effective care. Their initial partnership allowed them to collect extensive data and demonstrate the positive outcomes of their home care model.
As a result of their innovative approach and strategic partnerships, DispatchHealth has successfully expanded its services, continually transforming how high-acuity care is delivered.
DispatchHealth now provides a comprehensive home-based care system, offering services ranging from urgent and recovery care to population health management and hospital alternatives at home.
Challenges for Dispatch regarding reimbursement and scaling
In the early days, DispatchHealth faced numerous challenges. They had to navigate uncertainties about whether consumers truly wanted the convenience and different level of service in healthcare that DispatchHealth offered. Additionally, they needed to determine the scope of clinical care that could be safely and effectively delivered at home to drive the most value. There was also no payment model for the care that they were providing for commercial and medicare advantage.
From a business model perspective, scaling the operation also posed a significant challenge. Traditional healthcare facilities are efficient with patients coming to them, but DispatchHealth had to build a logistics platform to bring care directly to patients. This involved creating a technology-based healthcare logistics system that accounted for clinical acuity, as there was nothing off-the-shelf that met their needs.
Since there were no established payment models, initially they leveraged legacy house call codes provided by Medicare and partnered with local EMS agencies. By treating patients through the 911 system, they also could collect data and demonstrate the value of their services.
"We then took that data, based on the patients that we're treating out of the 911 system, and went back to the payers and said, 'Hey, we're seeing some of your members through the 911 system. We're taking care of them, we're avoiding an ambulance trip and we're avoiding an ER visit.”
DispatchHealth was able to track quality and utilization data for patients early on by being connected to a Health Information Exchange in Colorado.
This approach allowed them to negotiate rates with health insurance companies by showing they were avoiding ambulance trips and ER visits, tracking patients to ensure they stayed out of the emergency department, and ultimately proving the cost savings to payers.
By harnessing their partnership with the HIE, DispatchHealth gained access to vital data, empowering them to effectively negotiate rates with insurers while highlighting their proactive approach to patient care and cost reduction.
Securing Payer Contracts
DispatchHealth secured its initial payer contract with Anthem in Colorado, largely due to its roots as local clinicians with the right contacts in the local market. This local trust was crucial as payers are generally risk-averse and hesitant to adopt new care models that could disrupt their financial forecasts.
The early support from Anthem was instrumental, although securing subsequent contracts remained challenging. Despite Anthem's endorsement, expanding their network was a continuous uphill battle.
DispatchHealth expanded beyond Colorado in 2017, first targeting Phoenix, Arizona. This expansion required establishing entirely new contracts, despite some overlap in payer relationships.
“In each new state, we had to negotiate agreements with various types of plans, including Medicare Advantage, commercial plans, and managed Medicaid. Over time, DispatchHealth successfully formed national partnerships with major insurers such as United Healthcare, Humana, and Cigna and others.”
When considering geographic expansion, DispatchHealth didn't initially have a detailed, dialed in market growth strategy. Their decision to enter the Arizona market was driven by practical considerations, such as the high concentration of seniors and the feasibility of managing operations from Colorado. Some existing payer relationships also extended into Arizona, facilitating their entry into this market.
Another significant expansion occurred in 2017 into Richmond, Virginia. This move was catalyzed by recognition in the "Top 30 Startups to Know" list in Becker’s Hospital Review, which attracted the interest of the CEO of Bon Secours Richmond Health System. Bon Secours was transitioning to a value-based care model and saw potential in DispatchHealth's home-based care approach.
This partnership marked DispatchHealth's second significant health system collaboration and underscored the importance of strategic alliances in their expansion efforts.
In 2019, Dispatch was able to land and Optum/United National contract and by 2022 they secured an Anthem national and regional Blue contracts covering 22 states
The Patient Population and Provider Model for Dispatch
The patient population served by DispatchHealth encompasses a diverse range of individuals, with a notable focus on geriatric patients facing multiple comorbidities, being on multiple medications, and having mobility challenges.
These patients do not rely on urgent care but instead often rely on emergency room services due to their complex healthcare needs.
The average age of the patients served by DispatchHealth is around 62, indicating a significant skew towards the geriatric population. However, the organization also provides treatment for the pediatric population.
DispatchHealth recognizes the significance of this demographic, which constitutes a substantial portion of healthcare expenditure, particularly with approximately 65% of their patients falling under Medicare or Medicare Advantage coverage.
In addition, DispatchHealth's patient mix includes about 20% from commercial plans, 10% from managed Medicaid, and 5% from corporate accounts and self-pay.
They see significant potential in managed Medicaid due to rising populations and access issues.
For instance, in their Las Vegas market, partnering with Health Plan of Nevada (a United Healthcare subsidiary), they address primary care shortages by meeting patients at home within 24-72 hours post-hospital discharge.
This strategy ensures patients are on the right care path, have the necessary medications, and understand the importance of follow-up primary care appointments.
Regarding the provider side of their workforce, DispatchHealth initially leveraged relationships with experienced emergency room clinicians who were adept at handling acute medical conditions across all age groups.
When it comes to acute medical services, it is always difficult to predict the right demand of services in a given day. This is apparent in the ED where the general notion is that the busiest days for emergency rooms tend to be Mondays and weekends.
This trend is often due to people delaying seeking care over the weekend and a buildup of unmet medical needs by the start of the week.
"It is the exact same way for DispatchHealth. We wake up in the morning with no idea who will be reaching out to us or how many patients we will be seeing that day. In the early days, when we expanded outside of the 911 system, my co-founder and I answered the phones ourselves, hoping that individuals or provider organizations would contact us."
DispatchHealth has developed demand forecasting models to manage the supply and demand for acute visits effectively. They built these models by analyzing extensive data (internal and external data sets), including historical volume trends and seasonal patterns. By leveraging this data, DispatchHealth could closely track and predict volume trends similar to those observed in emergency rooms.
As they expanded into new markets and forged partnerships with community providers, home health agencies, health systems, and payers, DispatchHealth used these algorithms to anticipate service demand more accurately.
This predictive capability informed decisions about the necessary number of providers, vehicles, and team expansions. Additionally, the operational hours, consistently maintained from 8 AM to 10 PM daily, have been fine-tuned over the years to ensure they meet patient needs efficiently.
DispatchHealth faced significant challenges in getting patients to call and use their services. To overcome the perception of high costs and limited accessibility, they focused heavily on building strong community relationships.
Early on, they leveraged their network of partners and colleagues who worked closely with them in the healthcare trenches. By educating primary care physicians about their services, DispatchHealth positioned themselves as a viable alternative to the ER for patients needing immediate care when they couldn’t get timely appointments.
A crucial part of their strategy involved direct outreach. The founders and their team would visit practices, senior communities, and home health agencies during lunch hours to explain their services and build trust.
This hands-on, grassroots approach helped them gain traction in the market. Over time, as their reputation grew, they were able to train other team members to continue this outreach on their behalf, ensuring that more healthcare providers and patients became aware of and comfortable with using DispatchHealth’s services
Success of the DispatchHealth Model
"It's been incredibly gratifying over the last 10 years to see not just the data, but also the numerous patient stories we receive. We get calls from patients, provider organizations, and caregivers about the significant impact we have had on their lives. That's what keeps us going."
Since its inception, DispatchHealth has served over a million patients, accumulating extensive data on patient encounters. This data has consistently shown the company's success in achieving the Quadruple Aim, and even the Quintuple Aim, with a focus on health equity.
Their Net Promoter Score (NPS) has remained outstanding, with hundreds of thousands of reviews averaging a score of 98. To put this in perspective, healthcare organizations typically have an NPS of around 30, and even highly regarded companies like Apple average around 70.
DispatchHealth has excelled in providing a great experience from the initial contact to care delivery at home, and through to follow-up care. Their clinical outcomes have been impressive, notably achieving a 40% reduction in 30-day readmission rates for patients transitioning from the hospital.
This success extends across Medicare Advantage, commercial, and managed Medicaid plans, leading to significant cost savings.
On average, their pre-hospital care saves about $1,200 per episode, while their hospital-at-home model saves between $5,000 to $7,000 per episode.
These savings result from reduced DRG payments and substantial reductions in post-acute services and readmissions. Over the years, DispatchHealth has removed hundreds of millions of dollars from the healthcare system, showcasing their substantial impact.
DispatchHealth also strives for effective care coordination and interoperability with primary care providers.
This includes using various methods like sending faxes and partnering with Redox, an interoperability platform, to connect with Electronic Medical Record (EMR) systems.
Despite the challenges of using outdated technology like fax machines, they continue to find innovative ways to ensure seamless information flow and patient care continuity.
Partnership with Instacart
In 2024 and beyond, DispatchHealth is focused on execution and refining their operations to ensure continued growth and efficiency.
The company plans to expand selectively into new markets with strategic partners. Recently, they launched services in Minneapolis, Minnesota, in collaboration with Blue Cross Blue Shield of Minnesota.
Additionally, they have established an exciting partnership with MedStar Health in the Washington, DC market, enhancing their reach and impact in the region.
One of the notable developments for DispatchHealth is their recent partnership with Instacart to address food insecurity. This initiative stems from the understanding that when healthcare providers visit patients at home, they gain deeper insights into the patients' social determinants of health, such as nutrition and food availability.
Recognizing the significant impact of food insecurity on health outcomes, DispatchHealth is leveraging data collected from millions of patient encounters to connect individuals with the necessary resources.
Instacart's collaboration with DispatchHealth, which began in 2023, aims to identify patients facing food insecurity and link them with appropriate services.
DispatchHealth providers have the option to assign category-specific digital food allowances to patients via Instacart Health Fresh Funds, or arrange for food to be delivered directly to patients' homes with Care Carts.
Leveraging Instacart’s educational resources, DispatchHealth can also provide patients with personalized shopping lists via a tailored Virtual Storefront experience (source).
This partnership is particularly relevant as more Medicare Advantage plans adopt benefit structures to cover groceries and medically tailored meals. The initiative is still in its early stages, but it holds promise for improving patient health by ensuring access to nutritious food.
Additionally, this initiative empowers patients with actionable nutrition guidance and motivation, simplifying their journey towards improved health by encouraging an active role in their well-being through food.
Fundraising and Legal Insights for Founders
Today's fundraising environment is vastly different from what it was a few years ago. Founders should focus on securing good early adoption of their products or services and ensuring they have robust data to back up their claims.
This data is crucial for translating the value of the business to investors. It's also essential to have the right investors on your cap table—those who believe in your vision and will support you through the long journey.
This journey is not a short sprint but a long-term commitment, so having investors who understand and are committed to this process is vital.
When scaling a technology enabled provider organization, hiring / consulting with a competent healthcare regulatory attorney is critical due to the nuances of the regulatory environment, which can vary significantly from state to state.
It's important to conduct thorough due diligence in each state to ensure compliance with local regulations, understand what services can be provided by whom, and navigate reimbursement processes effectively.
Other key pieces of advice Kevin has:
Fail Fast: Quickly learn from failures and iterate on your business model or product.
Prudent Use of Capital: Manage your funding wisely to ensure it lasts as long as possible.
Provide Excellent Customer Service: Exceptional customer service, whether for consumers, partners, or internal teams, can significantly impact the success of the business.
Strive to be better every day: Even a mere 1% improvement, consistently pursued throughout your entire entrepreneurial journey, can yield remarkable impact and success.
"View your customers as part of your own team. Ensuring your customers and stakeholders are satisfied goes a long way and can lead to sustainable growth and success."
Interested in DispatchHealth? Learn more on their website, X, and LinkedIn
A note from our sponsor: Banc of California
Looking for guidance, connections, resources, opportunity? Banc of California’s banking products and services are built to support your evolving needs as you navigate the challenges of growing a successful business. As you continue to scale, our team will be with you every step of the way. Ready to take your business to the next level? Learn more:
https://bancofcal.com/